Epidemic of heat-related illnesses among workers exposed to hot working environments in the changing climate scenario
By Vidhya Venugopal, PK Latha, Tord Kjellstrom, Rebekah Lucas, Kristina Jakobsson, Jason Glaser, Seichi Horie, Marvin González-Quiroz, Sandra Peraza, Ilana Weiss, David Wegman, Theo Bodin, Cathrina Wessling, Hannu Rintamaki and Sirkka Rissanen, 12 April 2021
Research article
Rising global temperatures, coupled with decreasing access to clean drinking water, may enhance the effects of heat exposure to general and working populations across the globe. People working in jobs that require moderate or heavy manual labor in hot environments are at particular risk caused by the combined effect of exposures to high environmental heat and internal heat production. Exposures to heat can lead to a range of clinical health effects such as fatigue, exhaustion, heat syncope, fainting, heat stroke or even death. Furthermore, heat-related physical exhaustion leads to a reduction of the worker's ability to work with consequent productivity losses that may cause substantial economic losses for the businesses. The result of such continuous heat exposures, manual work and repeated dehydration are also known to cause acute kidney injuries that can further develop into chronic kidney diseases. With the predicted rise in temperatures due to climate change, the health effects for the working population are expected to become worse without appropriate interventions. With this background, the present review focuses on the heat-related health illnesses with special attention to kidney disease among workers engaged in manual physical labor in different occupational sectors.
Did you know how heat is affecting our body’s normal functioning?
The internal temperature of a healthy human body is maintained at around 37°C, and there are usually variations of less than 1°C that may occur depending on the level of physical activity or physical and psychological status and the time of the day. Any change in the body temperature that exceeds 1°C during a day occurs either due to illnesses or when the body is unable to cope with external temperatures. With a rise in environmental temperatures, it is natural that the body also tends to warm up. Normally, the body has ways of keeping itself cool, by letting heat escape through the skin, and by evaporating sweat (perspiration). The thermoregulatory mechanism tries to maintain a constant inner body temperature by pumping more blood to the extremities and also by increasing sweat production (figure 1). This helps the body to lose heat faster and maintain the thermal balance inside the body. In very hot environments, if the heat gain exceeds the heat loss, the body temperature begins to rise and if the body is not able to cool itself properly by external mechanisms, the exposed individual may suffer from heat stress followed by heat-related illness without appropriate interventions.
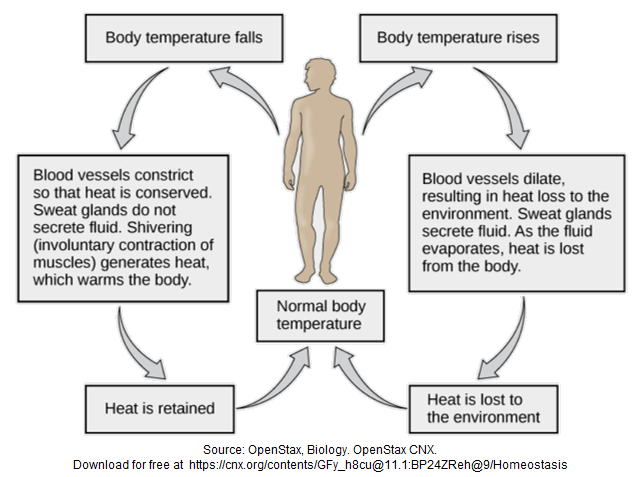
Figure 1. Thermal balance in humam body
Heat stress can induce heat illness at high temperatures during heavy manual work, influenced by the type of clothing being worn by the worker [OSHA, 2017]. The individual may at first be confused or unable to concentrate, followed by more severe symptoms, such as fainting or collapsing. Heat related illness can cause both direct or indirect health effects [R.S. Kovats and S. Hajat, 2008], the direct effects being a range of heat illness such as heat fatigue, heat rash, heat exhaustion to heat stroke. The indirect effects of heat stress could affect the body’s functioning via changes to the underlying physiological systems, which could result in other specific indicators such as renal insufficiency, acute cerebrovascular disease, and worsening of pulmonary disease [F.P. Ellis, 1976].
Heat-related illness usually comes in stages. The first stage is thirst, followed by muscle cramp, which can be mild or very painful. The more serious next stage of a heat-related illness (often called heat exhaustion) includes the individual having a cool, moist, pale skin, headache, dizziness and weakness, possible nausea and the skin may or may not feel hot [ACHD, 2018]. The warning signals and symptoms of the most serious stage of a heat-related illness, often called heat stroke or sun stroke, can vary between individuals and may include: vomiting, confusion, throbbing headache, high body temperature (as high as 40°C), reduction in alertness or loss of consciousness. The victim may stop sweating and the skin becomes red, hot and dry, but may still be moist with rapid, weak pulse, rapid, shallow breathing and/or seizures [A. Bouchama and J.P. Knochel, 2002]. Heat-related illnesses are most obvious for certain health outcomes such as renal and respiratory disease, especially in the elderly [R.S. Kovats et al., 2004].
Heat stress and its health risks
Many parts of the world have witnessed an increased number of heat waves and the number of people exposed to heatwaves increased by around 125 million [WHO, 2015; S. Rahmstorf and D. Coumou, 2011; Y. Sun et al., 2014], including India [S.K. Dash and A. Mamgain, 2011; K. Riahi et al., 2017; P. Rohini et al., 2016]. Between the years 1998 to 2017, more than 166,000 people died due to heatwaves that includes the 70,000 deaths during the 2003 heatwave in Europe. India documented 2,000 heat-related deaths between the years 2000-2016 as various parts of India experienced heatwaves [EMDAT, 2020]. It is well established that hot and humid work environments cause more serious problems to working people than a dry environment, as the high partial pressure of water vapor contained in the air in high humidity has a significant negative influence on the evaporative cooling and heat exchange conditions [A. Sobolewski et al., 2020]. In high humidity conditions, physical activity of the worker is possible only with additional or artificial cooling that increases the air flow.
Heat wave causes problems like heat stress, cardiovascular and respiratory disease, diarrhoeal disease, malnutrition and food insecurity, health impacts of extreme weather events, and occurrence of infectious disease [IPCC, 2014; WHO, 2003]. Among populations, the vulnerable are the affected the most, which includes old people, workers and people with pre-existing health conditions [S. Vandentorren et al., 2006]. Heat stress is a situation where too much heat is absorbed by a person, a plant or an animal and causes stress, illness or even death. Heat stress is identified by increase in body temperature, hot, dry skin, lack of sweating and neurological symptoms such as paralysis, headache, vertigo and unconsciousness. Exposed populations are at a risk of developing heat-related illnesses as heat affects them from the surrounding environment they live in [A. Bouchama et al., 2007; L.E. Thomas et al., 2010].
In India more than 20,000 people have died of heat-related causes since 1990 [S. Guleria and A.K. Gupta, 2018]. In 2010 and 2015, a total of 7,686 people lost their lives because of heat stroke, an average of more than 3 deaths per day [Dubbudu Rakesh, 2018]. Similarly in Arizona, one of the hottest places on earth, nearly 2,000 people visit local emergency rooms year after year due to heat-related illnesses. Deaths of children and elderly due to heat stroke during the heat waves were reported for 2003 and 2006 in [A. Fouillet et al., 2006] and for 2006 in [P. Empereur-Bissonnet et al., 2006]. The Center For Disease Control and Prevention (CDC) reported a total of 7,233 heat-related deaths in the U.S. between the years of 1999-2009. In that time, an average of 658 people died of heat-related causes each year [CDC, 2013]. People are less aware that direct thermal injury due to heat may also cause kidney tissue damage which leads to adverse renal issues [R.W. Schrier et al., 1970] as extreme heat exposure causes fluid loss, if severe, it may cause acute kidney injuries even in healthy individuals [M.A. Venkatachalam et al., 2010], let alone the workers laboring in hot environments. Apart from diabetes, hypertension, renal vascular disease and many other factors toxic to kidneys, the effect of heat stress on the kidney speeds up the kidney damage process [K. Patnala et al., 2014]. Over the past 10 years in the US, the Washington Post has reported 36 deaths and 2,810 heat-related illnesses on average each year [L. Bernstein, 2014]. However, officials from the Occupational Safety and Health Administration (OSHA) think that the true situation may be worse due to the lack of systematic autopsies and erroneous attribution of death to heart attacks. The Mercury California News reported two individuals – including a homeless man found dead in a car – have died from the heat in San Jose, Santa Clara County [G. Brassil, 2017].
Similarly the Indian newspaper Business Standard has reported that “In India extreme heat is already killing more people than reported. By 2030, it could also result in productivity loss equivalent to 34 million jobs and heat waves killed about 6,167 people in India over eight years to 2018” [B. Tripathi, 2020].
In 2012, 31 outdoor workers died in the heat and 4,120 fell ill, according to OSHA stats [L. Bernstein, 2014]. “Heat Kills: As temperatures climb, workers succumb to heat” – An article by Elizabeth Grossman on August 28, 2013 narrates the plight of James Baldasarre 45-year old, a Medford Massachusetts US Postal Service (USPS) employee who died of excessive heat had worked for USPS for 24 years who shortly before collapsing in the 35°C heat, texted his wife to say, “I’m going to die out here today. It’s so hot.” [E. Grossman, 2013] – proof of the importance of recognizing workers’ perceptions of heat stress impacts.
Are workers at higher risk?
Health risks during heat extremes are greater among people who are physically active (e.g. manual laborers, sports personnel etc.) [T. Kjellstrom et al., 2009; P.K. Nag et al., 2009]. According to the International Labour Organisation (ILO), too much heat in workplace can result in employees suffering the symptoms of heat-related illness.
Workdays spent outdoors in the heat and humidity is a fact of life for many laborers who are exposed to heat stress and consequent health risks. Heat-related illnesses potentially not only affect laborers who work outside, but also indoor industrial, factory and warehouse workers can be strongly affected by heat stress to temperature changes. Confined spaces, with the addition of appliances that generate heat, can just as easily mean that workers can be overheated and suffer exhaustion. Every year dozens of workers die and thousands more become ill while working in extreme heat or humid conditions in the US. More than 40 % of heat-related deaths at work occur in the construction industry, agriculture etc., but it does not exclude workers in other professions who are exposed to heat and are still susceptible to heat stress. A noticeable trend of rising in the number of heat-related illnesses and deaths in many cases due to rising temperatures is well documented. It has been linked to an increase in the greenhouse gas emissions due to industrialization that contributes to climate change [K. Smith et al., 2014; M.C. Sarofim et al., 2016].
Exposure to extreme heat presents a health hazard to all workers in low- and middle-income tropical countries who are involved in heavy physical work, working in strong light, and with minimal access to cooling systems while working [T. Kjellstrom et al., 2009]. Among the adverse heat-related health illnesses, occurrence of decreased renal functioning, acute kidney injuries, chronic kidney illnesses and kidney stones have been reported among the people working in extreme temperatures like steel manufacturing industry, agriculture etc. [L. Atan et al., 2005; L. Borghi et al., 1993; T.H. Brikowski et al., 2008; D.S. Raju et al., 2014]. It has also been found from studies conducted among sugarcane field workers engaged in manual work in hot and humid Nicaragua, El Salvador, Guatemala, Costa Rica etc., known as the sugar belt of Central America that workers are at a higher risk of renal diseases, including chronic kidney disease (CKD) [J. Glaser et al., 2016] (figure 2). A woman named Lakshmi from Balliputtuga, India has reported that in their village of less than 3,000 people, there are at least 126 widows due to chronic kidney disease of unknown etiology (CKDu). Many of their husbands were young agricultural workers who worked in the surrounding rice fields [isla network La, 2018]. Dr Joel Zapata, chief nephrologist of the hemodialysis wards in Piura and Sullana says that 30% of his dialysis patients are young men, 20-30 years old suffering from CKDu. “They arrive convulsing, vomiting and already at stage 5 kidney failure, never having shown symptoms before. Most come from the countryside and had worked in agriculture, fishing or on the docks.” [J. Roy et al., 2011]. In Central America, CKDu is a fatal progressive loss of kidney function that has killed more than 20,000 people in a single decade due to heat stress. A news paper release has shown that five men, all sugarcane workers and all sick with chronic kidney disease, were lying in hammocks outside the gates of the company in Chichigalpa, Nicaragua [isla network La, 2018]. In Sri Lanka’s North Central Province more than 23,500 people have died of CKDu, of which many of them are agricultural workers exposed to heat in their jobs [C. Jayasumana et al., 2016].

Figure 2. Nicaragua worker in hot sugarcane field
The issue is global – not local
Reports are pouring in from different parts of the world about the new epidemic of heat-related illnesses that are plaguing the tropics and especially the poor and vulnerable [L. Borghi et al., 1993; E. Hansen and M. Donohoe, 2003; B. Nielsen and P. Krog, 1994; S. Yamamoto et al., 2007]. Dr Vivekanand Jha from Delhi’s George Institute for Global Health said, “The increasing number of extreme heat waves due to global warming may disproportionately be causing kidney damage among at-risk populations” [S. Debroy, 2017]. But who is at higher risk? It is the poor and vulnerable, that includes the millions of workers across the globe, toiling in workplaces in spite of the hot weather? Based on the published reports and scientific literature between the last two decades, the issue seems to be growing in proportions that are not confined locally anymore and becoming a global issue. The map in figure 3 gives a snapshot of rising evidence among regions that have published heat studies also have studies on chronic kidney diseases as it is common to study issues that are of concern to the region. It has impacts on the families of the affected worker and also the businesses. The cost paid by the poor, vulnerable workers is not only health but economic losses due to their inability to work in hot conditions, consequent productivity losses, sickness and absenteeism, lost wages etc. [T. Kjellstrom et al., 2009]. This pushes them further into poverty as they lose their daily wages and even their jobs due to their inability to perform in heat [K. Lundgren et al., 2014]. In West Bengal state of India, Dr Shyamashree Dasgupta conducted an integrated economic analysis research study on heat stress and human welfare loss and the findings indicated that as humidity and temperature increase, productivity decreases. Climate Vulnerability Monitor, a report by DARA in 2012 calculated the economic losses due to climate change and the losses due to heat at work is estimated to be few trillion US dollars [DARA, 2012].
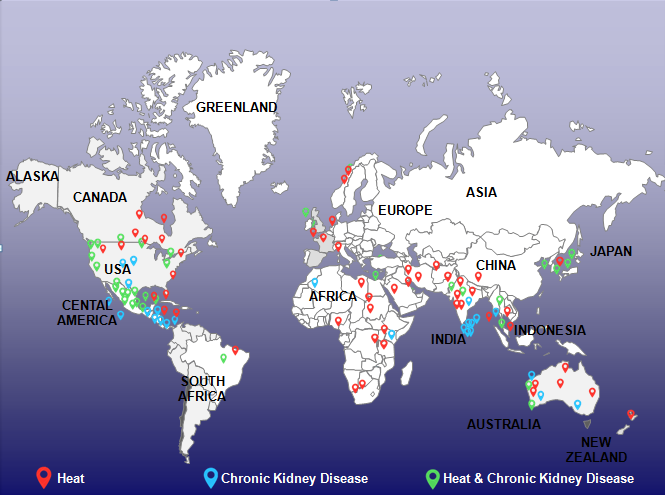
Figure 3. Global distribution of heat and chronic kidney diseases mapped based on published studies in these regions
The role of climate change
In the last 100 years, the mean global average surface temperature has increased about 0.74°C. Over the past 50 years, more widespread changes in extreme temperatures and rain have been reported and the rate of change has increased over time [IPCC, 2007]. It is estimated that it will go up a further 1.8–4.0°C (estimated average 3.0°C) by 2100 [IPCC, 2007]. This rise in temperature leads to heat waves [S. Hajat et al., 2006] that cause distress to the human population. Climate change is happening and progressing at a rate that already has adverse effects on the ecosystem and people’s health worldwide [IPCC, 2014]. With rising temperatures, the heat stress imposed on the workers is expected to become much worse [V. Venugopal et al., 2015] and with consequent additional burden of health risks. Times of India, a premier newspaper in India has identified drought-hit villages across Maharashtra grapple with an increased incidence of kidney stones [S. Debroy, 2017]. Another new multi-centric study has claimed that climate change could lead to an epidemic of chronic kidney disease [S. Debroy, 2017]. Similarly an article in the Clinical Journal of the American Society of Nephrology said there is likely to be water shortages that could further cause dehydration and heat stress, which could affect kidneys [V. Jha, 2016]. The consequence of not taking action now by adopting preventive and adaptive strategies to combat heat at work in the changing climate scenario, may be a generation of unhealthy workers and economic losses for the country.
Conclusion
Climate change will create a variety of direct and indirect occupational health hazards. These include effects of environmental heat, injuries during extreme weather events, risks of vector-borne diseases, and other indirect effects as the climate is changing. The most prominent hazard is heat stress as it touches all lives and there is an urgent need for health researchers to identify work practices that contribute to heat-related illnesses. Efforts to test targeted, robust prevention strategies for preventing occupational heat stress especially in developing countries which requires a concerted multidisciplinary effort from engineers, employers, health authorities, researchers, and governments. Proper planning, inter-sectoral dialogues and coordinated efforts between various stakeholders may help avert the damages to workers and face the hotter world as climate change proceeds.
- ACHD: Heat-Related Illnesses: A Factsheet. Allegheny County Health Department. Retrieved (6 2018) from http://www.achd.net/factsheet/heat.html.
- L. Atan, C. Andreoni, V. Ortiz, E.K. Silva, R. Pitta, F. Atan and M. Srougi: High kidney stone risk in men working in steel industry at hot temperature, Urology, vol. 65, 858-61, https://doi.org/10.1016/j.urology.2004.11.048, 2005.
- L. Bernstein (07 07 2014): American workers die needlessly in the heat every year, Washington Post. Retrieved from https://www.washingtonpost.com/news/to-your-health/wp/2014/07/07/american-workers-die-needlessly-in-the-heat-every-year/.
- L. Borghi, T. Meschi, F. Amato, A. Novarini, A. Romanelli and F. Cigal: Hot occupation and nephrolithiasis, The Journal of urology, vol. 150, 1757-60, https://doi.org/10.1016/S0022-5347(17)35887-1, 1993.
- A. Bouchama, M. Dehbi, G. Mohamed, F. Matthies, M. Shoukri and B. Menne: Prognostic factors in heat wave–related deaths: a meta-analysis, Archives of internal medicine, vol. 167, 2170-6, https://doi.org/10.1001/archinte.167.20.ira70009, 2007.
- A. Bouchama and J.P. Knochel: Heat Stroke, New England Journal of Medicine, vol. 346, 1978-1988, https://doi.org/10.1056/NEJMra011089, 2002.
- G. Brassil (21 06 2017): Two people dead in San Jose from the heat, The Mercury News. Retrieved from https://www.mercurynews.com/2017/06/21/two-san-jose-residents-died-from-heat-stroke/.
- T.H. Brikowski, Y. Lotan and S. Pearle: Climate-related increase in the prevalence of urolithiasis in the United States, in: Proceedings of the National Academy of Sciences, 9841-6, 2008.
- CDC: Heat-Related Deaths After an Extreme Heat Event — Four States, 2012, and United States, 1999–2009, Morbidity and Mortality Weekly Report, Centers for Disease Control and Prevention, 2013. Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6222a1.htm.
- DARA: Climate Vulnerability Monitor 2nd Edition: A Guide to the Cold Calculus of a Hot Planet, DARA and the Climate Vulnerable Forum, 2012.
- S.K. Dash and A. Mamgain: Changes in the frequency of different categories of temperature extremes in India, Journal of Applied Meteorology and Climatology, vol. 50, 1842-58, https://doi.org/10.1175/2011JAMC2687.1, 2011.
- S. Debroy (01 04 2017): Heat stroke deaths in Maharashtra rising; 33 lose lives in past four years, The Times of India. Retrieved from https://timesofindia.indiatimes.com/city/mumbai/heat-stroke-deaths-in-maha-rising-33-lose-lives-in-past-four-years/articleshow/57949585.cms.
- F.P. Ellis: Heat Illness. II Pathogenesis, Transactions of the royal society of tropical medicine and hygiene, vol. 70, 412-18, https://doi.org/10.1016/0035-9203(76)90121-8, 1976.
- EMDAT: The International Disaster Database. Retrieved (2020) from https://www.emdat.be.
- P. Empereur-Bissonnet, G. Salines, B. Berat, N. Caillere and L. Josseran: Heatwave in France, July 2006: 112 Excess Deaths So Far Attributed to the Heat, Eurosurveillance, vol. 11, https://doi.org/10.2807/esw.11.31.03014-en, 2006.
- A. Fouillet, G. Rey, F. Laurent, G. Pavillon, S. Bellec, C.J. Clavel, E. Jougla and D. Hémon: Excess Mortality Related to the August 2003 Heat Wave in France, International archives of occupational and environmental health, vol. 80, 16-24, https://doi.org/10.1007/s00420-006-0089-4, 2006.
- J. Glaser, J. Lemery, B. Rajagopalan, H.F. Diaz, R. García-Trabanino, G. Taduri, M. Madero, M. Amarasinghe and and co-authors: Climate Change and the Emergent Epidemic of Chronic Kidney Disease (CKD) from Heat Stress in Rural Communities: The Case for Heat Stress Nephropathy, Clinical Journal of the American Society of Nephrology, vol. 11, 1472-83, https://doi.org/10.2215/CJN.13841215, 2016.
- E. Grossman (28 08 2013): Heat Kills: As temperatures climb, workers succumb to heat, The Pump Handle, Public Health Practice. Retrieved from http://www.thepumphandle.org/2013/08/28/heat-kills-as-temperatures-climb-workers-succumb-to-heat/.
- S. Guleria and A.K. Gupta: Heat Wave in India Documentation of State of Telangana and Odisha (2016), National Institute of Disaster Management, New Delhi., 124 pp., 2018. Retrieved from https://nidm.gov.in/PDF/pubs/heat_wave_18.pdf.
- S. Hajat, B. Armstrong, M. Baccini, A. Biggeri, L. Bisanti, A. Russo, A. Paldy, B. Menne and T. Kosatsky: Impact of high temperatures on mortality: is there an added heat wave effect?, Epidemiology, vol. 17, 632-8, https://doi.org/10.1097/01.ede.0000239688.70829.63, 2006.
- E. Hansen and M. Donohoe: Health issues of migrant and seasonal farmworkers, Journal of Health care for the Poor and Underserved, vol. 14, 153-164, https://doi.org/10.1353/hpu.2010.0790, 2003.
- IPCC: Climate Change 2007: The Physical Science Basis. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change, S. Solomon, D. Qin, M. Manning, Z. Chen, M. Marquis, K.B. Averyt, M. Tignor and H.L. Miller (Eds.). Cambridge University Press, 2007.
- IPCC: Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change, C.B. Field, V.R. Barros, D.J. Dokken, K.J. Mach, M.D. Mastrandrea, T.E. Bilir, M. Chatterjee, K.L. Ebi, Y.O. Estrada and co-editors (Eds.). Cambridge University Press, 1132 pp., 2014.
- C. Jayasumana, C. Orantes, R. Herrera, M. Almaguer, L. Lopez, L.C. Silva, P. Ordunez, S. Siribaddana and and co-authors: Chronic Interstitial Nephritis in Agricultural Communities: A Worldwide Epidemic with Social, Occupational and Environmental Determinants, Nephrology Dialysis Transplantation, vol. 32, 234-41, https://doi.org/10.1093/ndt/gfw346, 2016.
- V. Jha: Climate change may be causing chronic kidney disease by triggering dehydration and heat stress. The George Institute for Global Health India. Retrieved (11 05 2016) from https://www.georgeinstitute.org.in/media-releases/climate-change-may-be-causing-chronic-kidney-disease-by-triggering-dehydration-and.
- T. Kjellstrom, I. Holmer and B. Lemke: Workplace heat stress, health and productivity–an increasing challenge for low and middle-income countries during climate change, Global Health Action, vol. 2, https://doi.org/10.3402/gha.v2i0.2047, 2009.
- R.S. Kovats and S. Hajat: Heat Stress and Public Health: A Critical Review, Annual Review of Public Health, vol. 29, 41-55, https://doi.org/10.1146/annurev.publhealth.29.020907.090843, 2008.
- R.S. Kovats, S. Hajat and P. Wilkinson: Contrasting Patterns of Mortality and Hospital Admissions During Hot Weather and Heat Waves in Greater London, UK, Occupational and environmental medicine, vol. 61, 893-98, https://doi.org/10.1136/oem.2003.012047, 2004.
- isla network La: Balliputuga, India – The Other Island of Widows. Retrieved (06 2018) from https://laislanetwork.org/portfolio-items/balliputuga/?portfolioCats=64%2C63%2C67%2C69%2C68.
- K. Lundgren, K. Kuklane and V. Venugopal: Occupational heat stress and associated productivity loss estimation using the PHS model (ISO 7933): a case study from workplaces in Chennai, India, Global Health Action, vol. 7, https://doi.org/10.3402/gha.v7.25283, 2014.
- P.K. Nag, A. Nag, P. Sekhar and S. Pandit: Vulnerability to Heat Stress: Scenario in Western India, National Institute of Occupational Health, Ahmedabad, 2009.
- B. Nielsen and P. Krog: Optimal Fluid Replacement During Long‐Lasting Exercise in 18° C and 32° C Ambient Temperature, Scandinavian journal of medicine and science in sports, vol. 4, 173-80, https://doi.org/10.1111/j.1600-0838.1994.tb00422.x, 1994.
- OSHA: Technical Manual on Health Hazards. Occupational Safety and Health Administration. Retrieved (9 2017) from https://www.osha.gov/dts/osta/otm/otm_iii/otm_iii_4.html.
- K. Patnala, D.S.S.K. Raju and K.V. Rachel: Climate Change And Chronic Kidney Disease, Asian Journal of Pharmaceutical and Clinical Research, vol. 7, 2014.
- S. Rahmstorf and D. Coumou: Increase of extreme events in a warming world, in: Proceeding of the National Academy of Sciences of the United States of America, 17905-17909, 2011.
- D.S. Raju, P. Kiranmayi and K.V. Rachel: Climate change and chronic kidney disease, Asian Journal of Pharmaceutical and Clinical Research, vol. 7, 53-7, 2014.
- Dubbudu Rakesh (07 03 2018): 1 out of every 5 Heat Stroke deaths in India occurs in Andhra Pradesh, FACTLY. Retrieved from https://factly.in/1-every-5-heat-stroke-deaths-india-occurs-andhra-pradesh/.
- K. Riahi, D.P.V. Vuuren, E. Kriegler, J. Edmonds, B.C. O’Neill, S. Fujimori, N. Bauer, K. Calvin and and co-authors: The Shared Socioeconomic Pathways and Their Energy, Land Use, and Greenhouse Gas Emissions Implications: An Overview, Global Environmental Change, vol. 42, 153-68, https://doi.org/10.1016/j.gloenvcha.2016.05.009, 2017.
- P. Rohini, M. Rajeevan and A.K. Srivastava: On the variability and increasing trends of heat waves over India, Scientific reports, vol. 19, https://doi.org/10.1038/srep26153, 2016.
- J. Roy, A. Chakrabarty, K. Mukhopadhyay and M. Kanjilal: Climate Change, Heat Stress and Loss of Labour Productivity: A Method for Estimation, Indian Society for Ecological Economics (INSEE) Biennial Conference, Hyderabad (2011)
- M.C. Sarofim, S. Saha, M.D. Hawkins, D.M. Mills, J. Hess, R. Horton, P. Kinney, J. Schwartz and A. St-Juliana: Ch. 2: Temperature‐related death and illness, in: The impacts of climate change on human health in the United States: A scientific assessment. U.S. Global Change Research Program, Washington, DC, 43-68, https://doi.org/10.7930/J0MG7MDX, 2016.
- R.W. Schrier, J. Hano, H.I. Keller, R.M. Finkel, P.F. Gilliland, W.J. Cirksena and P.E. Teschan: Renal, metabolic, and circulatory responses to heat and exercise: Studies in military recruits during summer training, with implications for acute renal failure, Annals of internal medicine, vol. 73, 213-23, https://doi.org/10.7326/0003-4819-73-2-213, 1970.
- K. Smith, A. Woodward, D. Campbell-Lendrum, D. Chadee, Y. Honda, Q. Liu, J. Olwoch, B. Revich, R. Sauerborn and co-authors: Human health: impacts, adaptation, and co-benefits, in: Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change, C.B. Field, V.R. Barros, D.J. Dokken, K.J. Mach, M.D. Mastrandrea, T.E. Bilir, M. Chatterjee, K.L. Ebi, Y.O. Estrada and co-editors (Eds.). Cambridge University Press, 709-754, 2014.
- A. Sobolewski, M. Młynarczyk, M. Konarska and J. Bugajska: The influence of air humidity on human heat stress in a hot environment, International Journal of Occupational Safety and Ergonomics0, 1-11, https://doi.org/10.1080/10803548.2019.1699728, 2020.
- Y. Sun, X. Zhang, F.W. Zwiers, L. Song, H. Wan, T. Hu, H. Yin and G. Ren: Rapid increase in the risk of extreme summer heat in Eastern China, Nature Climate Change, vol. 4, https://doi.org/10.1038/nclimate2410, 2014.
- L.E. Thomas, R.D. Dear, R. Rawal, A. Lall and P. Thomas: Air Conditioning, Comfort and Energy in India’s Commercial Building Sector, Windsor Conference on Thermal Comfort, Network for Comfort and Energy Use in Buildings (NCEUB) (2010)
- B. Tripathi (20 06 2020): Vulnerable to rise in temperature, India needs to take heatwave seriously, Business Standard. Retrieved from https://www.business-standard.com/article/current-affairs/vulnerable-to-rise-in-temperature-india-needs-to-take-heatwave-seriously-120062001309_1.html.
- S. Vandentorren, P. Bretin, A. Zeghnoun, L. Mandereau-Bruno, A. Croisier, C. Cochet, J. Ribéron and and co-authors: August 2003 heat wave in France: risk factors for death of elderly people living at home, The European Journal of Public Health, vol. 16, 583-591, https://doi.org/10.1093/eurpub/ckl063, 2006.
- M.A. Venkatachalam, K.A. Griffin, R. Lan, H. Geng, P. Saikumar and A.K. Bidani: Acute kidney injury: a springboard for progression in chronic kidney disease, American Journal of Physiology-Renal Physiology, vol. 298, 1078-94, https://doi.org/10.1152/ajprenal.00017.2010, 2010.
- V. Venugopal, J.S. Chinnadurai, R.A.I. Lucas and T. Kjellstrom: Occupational Heat Stress Profiles in Selected Workplaces in India, International journal of environmental research and public health, vol. 13, https://doi.org/10.3390/ijerph13010089, 2015.
- WHO: Climate change and human health: risks and responses, A.J. McMichael, D.H Campbell-Lendrum, C.F. Corvalan, K.L. Ebi, A.K. Githeko, J.D. Scheraga and A. Woodward (Eds.). World Health Organization, 2003.
- WHO: Health Topics / Heatwaves. Retrieved (2015) from https://www.who.int/health-topics/heatwaves#tab=tab_1/.
- S. Yamamoto, M. Iwamoto, M. Inoue and N. Harada: Evaluation of the effect of heat exposure on the autonomic nervous system by heart rate variability and urinary catecholamines, Journal of occupational health, vol. 49, 199-20429, https://doi.org/10.1539/joh.49.199, 2007.
